In the 21st century, women are more empowered, educated, and ambitious than ever before. They’re building careers, managing households, caring for families, staying socially connected, and striving for personal fulfillment—all at once. Yet beneath this progress lies a growing, often unspoken challenge: chronic stress and burnout and their profound impact on female fertility.
Many women who struggle to conceive are told to focus on age, hormones, or genetics. What’s discussed far less openly is the invisible load women carry every day—the mental, emotional, and physical stress that quietly disrupts reproductive health. Stress doesn’t just affect mood or sleep; it can interfere with ovulation, hormone balance, menstrual cycles, and even implantation.
This article explores how stress and burnout affect fertility, why modern women are especially vulnerable, the science behind the connection, and—most importantly—what can be done to restore balance and support reproductive health.
Understanding Stress and Burnout in Modern Women
Stress is no longer an occasional response to a challenge; for many women, it’s a constant state. Emails never stop, work bleeds into personal time, and societal expectations continue to rise. Burnout occurs when this prolonged stress overwhelms the body’s ability to recover.
Burnout isn’t just feeling tired—it’s a state of emotional exhaustion, mental overload, and physical depletion. Women experiencing burnout often report feeling numb, disconnected, irritable, or chronically fatigued. These symptoms may seem unrelated to fertility at first glance, but the body doesn’t compartmentalize stress. What affects the mind inevitably affects the reproductive system.
Modern stressors are uniquely intense. Unlike acute stress—such as a short-term deadline—chronic stress keeps the nervous system in a constant “fight or flight” mode. Over time, this state signals to the body that survival is the priority, not reproduction.
Why Women in the 21st Century Are More Stressed Than Ever
Women today face a convergence of pressures that previous generations experienced separately.
Career demands are higher, especially in competitive or male-dominated industries. Many women delay motherhood to establish financial stability, yet face anxiety about fertility decline as they age. Social media adds another layer—constant comparison, unrealistic standards, and the pressure to “have it all” without showing struggle.
Additionally, women still shoulder the majority of emotional labor—planning, organizing, caregiving, and maintaining relationships. Even when responsibilities are shared, the mental load often isn’t. Over time, this invisible labor accumulates, leading to exhaustion and hormonal disruption.
The irony is painful: women are doing everything “right,” yet their bodies may quietly signal distress through missed periods, irregular cycles, or difficulty conceiving.
The Science: How Stress Affects Female Fertility
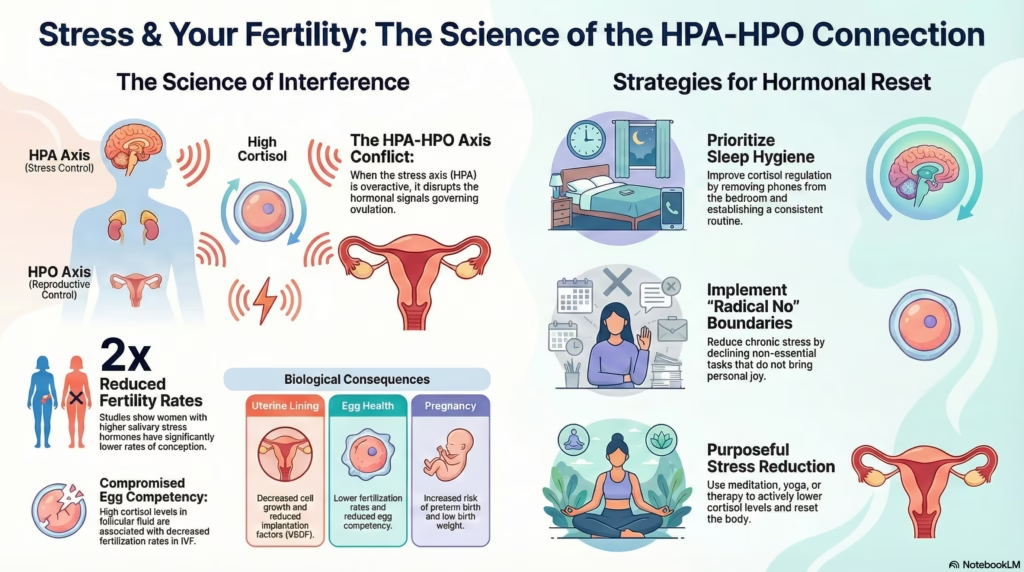
Stress impacts fertility through multiple interconnected biological pathways. At the center is the hypothalamic-pituitary-adrenal (HPA) axis, the system that controls the stress response.
When stress is chronic, the body releases elevated levels of cortisol. While cortisol is essential in short bursts, prolonged elevation disrupts communication between the brain and ovaries. This can suppress the release of gonadotropin-releasing hormone (GnRH), which is necessary for ovulation.
In simple terms: when the body perceives constant stress, it may delay or shut down reproductive processes as a protective mechanism.
Stress can lead to:
- Irregular or absent ovulation
- Shortened or disrupted luteal phase
- Changes in cervical mucus
- Reduced egg quality over time
- Lower implantation rates
Stress also increases inflammation and oxidative stress, both of which negatively affect fertility and early pregnancy.
Burnout, Hormones, and the Menstrual Cycle
Hormones operate in a delicate balance. Chronic stress throws this balance off.
Elevated cortisol competes with progesterone, a hormone essential for ovulation, implantation, and maintaining early pregnancy. This imbalance can result in:
- Short cycles
- Premenstrual spotting
- Worsened PMS
- Luteal phase defects
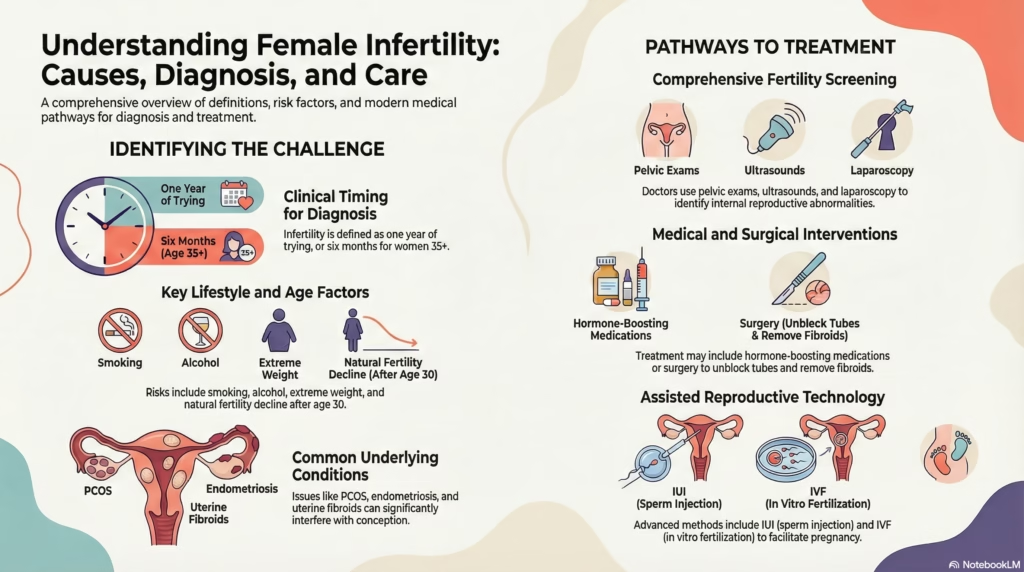
Stress can also worsen conditions such as polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, and endometriosis—each of which already poses fertility challenges.
For many women, burnout manifests as cycle irregularity long before fertility issues are formally diagnosed.
The Emotional Toll of Fertility Struggles
Fertility challenges don’t exist in a vacuum. They often amplify stress, creating a vicious cycle: stress affects fertility, fertility struggles increase stress.
Women may experience:
- Guilt or self-blame
- Anxiety around timing, ovulation, or test results
- Depression or emotional numbness
- Isolation, especially when peers conceive easily
Because fertility struggles are deeply personal, many women suffer in silence. Society celebrates pregnancy announcements but rarely creates space for grief, uncertainty, or waiting.
This emotional burden further dysregulates the nervous system, making relaxation—an essential component of fertility—feel impossible.
Workplace Culture and Fertility Stress
Modern work culture often glorifies overachievement and constant availability. Long hours, shift work, lack of rest, and job insecurity all contribute to reproductive stress.
Women may feel forced to choose between career progression and fertility treatments. Time off for appointments, injections, or recovery can feel like a liability. The result is suppressed needs and heightened anxiety.
Research has shown that women with high job strain may experience:
- Longer time to conception
- Increased risk of menstrual irregularities
- Higher miscarriage risk
A culture that ignores biological limits inadvertently undermines women’s reproductive health.
Lifestyle Stressors That Quietly Impact Fertility
Beyond emotional stress, modern lifestyles introduce additional fertility stressors:
- Poor sleep from screen exposure and irregular schedules
- Over-exercising driven by body image pressure
- Under-eating or restrictive dieting
- Caffeine and alcohol dependence
- Constant digital stimulation
Individually, these may seem manageable. Together, they keep the nervous system overstimulated and the body depleted.
Fertility thrives in an environment of safety, nourishment, and rest—conditions many modern women struggle to achieve.
Can Reducing Stress Really Improve Fertility?
While stress is not the sole cause of infertility, evidence suggests that addressing it can significantly improve reproductive outcomes.
Studies have shown that women who engage in stress-reduction practices—such as mindfulness, yoga, counseling, or cognitive behavioral therapy—often experience improved ovulation, cycle regularity, and pregnancy rates, including during assisted reproductive treatments.
Reducing stress doesn’t mean eliminating ambition or responsibility. It means teaching the body that it is safe enough to reproduce.
Practical Ways to Support Fertility While Managing Stress
Supporting fertility in a high-stress world requires intentional shifts, not perfection.
Helpful strategies include:
- Prioritizing sleep as a non-negotiable
- Eating enough calories and nutrients to support hormone production
- Gentle movement over punishing exercise
- Setting boundaries around work and digital consumption
- Practicing nervous system regulation (breathing, meditation, time in nature)
- Seeking emotional support through therapy or support groups
Even small changes can signal safety to the body over time.
Reframing Fertility: It’s Not a Personal Failure
One of the most damaging aspects of fertility struggles is the belief that the body is “failing.” In reality, the body is often responding intelligently to prolonged stress.
Fertility is not just about reproductive organs—it’s about overall health, safety, and balance. When stress is addressed with compassion rather than pressure, the body often responds positively.
Modern women don’t need more discipline. They need more support.
When to Seek Professional Help
If stress feels unmanageable or fertility challenges persist, professional support can be transformative.
Consider seeking help if you experience:
- Persistent cycle irregularities
- Amenorrhea (missing periods)
- Severe PMS or hormonal symptoms
- Ongoing anxiety or depression
- Difficulty conceiving after 6–12 months
A holistic approach—addressing both emotional and physical health—often yields the best outcomes.
Conclusion: Breaking the Silence Around Stress and Fertility
Stress, burnout, and fertility are deeply intertwined, yet rarely discussed together. Modern women are navigating unprecedented demands while expecting their bodies to function optimally under pressure.
By acknowledging the impact of stress on fertility, we move away from blame and toward understanding. Supporting reproductive health means supporting the whole woman—her mind, body, and emotional well-being.
Fertility isn’t just about timing or tests. It’s about creating space for rest, safety, and healing in a world that rarely slows down.

Dr. Mamta Pattnayak is working as a Additional Director in Gynae and Obstetrics Dept. in Fortis Hospital, Gurgaon. Dr. Mamta Pattnayak is an MBBS graduate from S.C.B. Medical College, Cuttack and completed her MD (Obstetrics & Gynaecology) from Sambalpur University in 2003. With a rich experience of over years to her credit, Dr. Mamta has undergone training on advance lap Gynae by Ethicon. Done hand’s on Colposcopy course by RCOG. She is certified as a mentor in RCOG training course in Max Hospital Saket. Dr. Mamta has been associated with several organizations like Moolchand Hospital, New Delhi besides others. Her last assignment was at Max Super Specialty Hospital, Saket, New Delhi. Recently she has also started her private clinic at: Mother’s Touch HealthCare Centre: 395P, Sector 39 Rd, opposite to Medanta Hospital, near Gurudwara, Sector 39, Gurugram, Haryana 122004


